

Living Our Mission in a Defining Year
For BlueCross BlueShield of Tennessee, the clock both stopped and started in March 2020 as we took extraordinary measures to respond to the COVID-19 public health crisis.
We stopped any semblance of business as usual and immediately started transforming BlueCross BlueShield of Tennessee to benefit our members and our TeamBlue employees.
While the health care industry responded quickly and with overwhelming commitment to the health emergency, the virus has claimed the lives of far too many people across the state. Among them are plan members we’ve served, as well as cherished relatives, coworkers and friends.
Overnight, we transitioned to an innovative new work model, implemented a series of industry-changing actions that created immediate access to care. We also rapidly began delivering more than $9 million in support for affected communities and families statewide through our BlueCross Foundation.
The year 2020 proved to be our once-in-a-generation test to truly live our mission – in a by taking swift actions to enhance our ability to protect our members’ health, shield our own employees, and quickly and confidently choose the right thing to do – in a time of daunting challenge.
Our members always need us, but in 2020 depended on us more than ever. And combined with the national requisite for racial justice and healing, the need was great.
First Major Insurer to Lead with Telehealth
We became the first major insurer to commit to covering in-network telehealth services on an ongoing basis. In short time, by partnering with our providers, we saw 80 times more telemedicine claims than during the same period the previous year – an outstanding increase in access for our members.
Real Relief for Members, Groups and Providers
We made the decision early on to immediately waive member costs on COVID-19 testing and treatment until the end of the COVID-19 national emergency – whenever that may be. And later, for the approved and fast-tracked vaccines. We waived primary care and behavioral health costs for our Medicare Advantage members – those most vulnerable to the pandemic.
We also moved swiftly to assist our customer groups by extending payment periods to help their employees keep their critical group coverage – even as so many small businesses were facing difficult decisions about mass layoffs and closures.
And we honored and supported the front-line providers and first responders who worked tirelessly to deliver care round the clock.
Excelling in Member Satisfaction
Through the end of the year, our net promoter score continued to rise as our levels of service only increased during the challenging period. As an indicator of outstanding member satisfaction and loyalty, we’re working to be in the top quartile of performance for this key consumer service metric.
Taking the Right and Only Stand Against Racism
Though separated by distance, we joined together in our support of racial justice and healing, establishing internal conversations to make sure our employees had the opportunity to speak of their experiences, and taking the conversation public with a stake-in-the-ground stance against racism.
Our Mission is Our Guide
Throughout 2020, we took care with each decision to ensure it was the right thing to do for our members, our groups, and the providers we rely on to care for BlueCross members – to deliver peace of mind through better health, and an unqualified level of support in a defining moment of challenge and change.
JD Hickey, M.D.
President and CEO
Marty G. Dickens
Chairman of the Board
Making COVID-19 Relief a Reality
The health of our members, employees and the communities we serve was the first priority in 2020. Since the COVID-19 pandemic was unlike anything we had faced, our first decision was to remove any barriers to those needing and receiving care. We waived all member cost-sharing for COVID-19 treatments, including hospitalizations, in addition to waiving copays and cost-sharing for FDA-approved COVID-19 testing. No out-of-pocket costs were necessary for testing and treatment administered through in-network providers, including care at a doctor’s office, urgent care facility, emergency room, and COVID-19-related inpatient hospital stays.
As COVID-19 made its way to Tennessee, BlueCross took immediate steps to prepare for and respond to member and community needs, including supporting providers and first responders who placed their lives on the line every day. Our nurses and case managers took additional measures to ensure members had both their health and safety needs met – even arranging for food pantry and meal deliveries for those having financial difficulties.
BlueCross Foundation provided almost $9 million to support area food banks, sponsor provider education and COVID-19 vaccine education, address health disparities and encourage vaccine acceptance – especially in communities of color. And though in-person volunteer activities were suspended temporarily in 2020 due to COVID-19, TeamBlue volunteers still found ways to help their neighbors through our Community Trust outreach and engagement opportunities, making personal calls and check-ins on area residents as an additional way to give back to the communities where they live and work.
There were many ways to say thank you to the first responders and health care professionals who stepped up to the challenge and remained in action throughout the most difficult times of the coronavirus outbreak. BlueCross chose to thank and recognize the doctors, nurses, firefighters, police officers and EMTs for their life-saving work with public ad messages, social media support, and more than 6,500 yard signs that every employee could place in on their property. The signs and messaging – along with donating and delivering lunchtime meals to hospital work teams across the state – were a unifying way for BlueCross, our employees and volunteers, to visibly show support for these heroic efforts.
We became the first major insurer to embrace telehealth for the long-term after our dramatic expansion of these services during the COVID-19 pandemic. Strategically aligning with our commitment to improve access to primary care, our decision to permanently cover virtual visits with in-network providers gave members easier access and options to health care services moving forward. Our decision covered telephone and video visits with primary care providers, specialists, and behavioral health providers, as well as occupational, physical, speech, and ABA therapy services. Telehealth offers members and their trusted providers more options that fit their everyday needs for preventive, routine and maintenance care – driving better health.
Primary care is one of the best ways a person can pursue better health – and BlueCross BlueShield of Tennessee has a history of investing in successful, collaborative partnerships to elevate and ensure quality primary care for statewide residents. Our joint venture to open eight primary care clinics with Sanitas, a Keralty company, demonstrated an innovative way to fulfill our 2020 business priority to advance new models of care. Supporting and expanding convenient access to primary care, these medical centers in Middle and West Tennessee exclusively serve BlueCross members from all lines of business, along with self-pay and original Medicare members. Benefits of using our new clinics include same-day appointments, extended hours, and enhanced digital tools that make it easy to connect with care teams and medical center staff.
For the sixth year in a row, CMS recognized our Medicare Advantage PPO plan with a 4-Star quality achievement rating. Never easy to achieve, this industry accolade is based on up to 40 different performance measures, which are updated and weighted differently each year. Measures and calculation points can also change annually based on other Medicare Advantage plans’ performance across the U.S. – as well as CMS Stars program changes – so the bar continues to be raised each year. Four-Star rankings require consistent high performance across the entire structure of plan operations – with metrics designed to continually push plan programs for continuous improvement.
For all the progress made, the scars of deep-seated racism still exist. The disparities evident in COVID-19 outcomes and several tragic deaths over the summer turned our collective eyes to these issues with a new sense of urgency. We made a public statement to work to end racism and committed the company to better serve our communities in support of these specific needs. We funded new ventures and partnerships to research and address health disparities and hosted our most-attended Power of We workforce diversity conference to share best practices with business leaders across the state.
At the start of 2020, no one could have predicted that 97% of our employees would spend the next year working from their homes – or that we’d have to make the transition happen in a matter of days. Change has become the new normal and BlueCross BlueShield of Tennessee has adapted well to change over the past decade, as the competitive marketplace and regulatory landscape have evolved. Throughout, our enterprise strategy has focused on helping employees tie their roles and impact to our strategic goals, aligning our efforts while building agility and resilience. When faced with the need to balance the health of our employees and our commitment to member service, we were ready. In an unplanned era of remote work, our people have thrived – maintaining high levels of service, collaborating in new ways, and increasing our already-high engagement scores.


Living Our Mission in a Defining Year
For BlueCross BlueShield of Tennessee, the clock both stopped and started in March 2020 as we took extraordinary measures to respond to the COVID-19 public health crisis.
We stopped any semblance of business as usual and immediately started transforming BlueCross BlueShield of Tennessee to benefit our members and our TeamBlue employees.
While the health care industry responded quickly and with overwhelming commitment to the health emergency, the virus has claimed the lives of far too many people across the state. Among them are plan members we’ve served, as well as cherished relatives, coworkers and friends.
Overnight, we transitioned to an innovative new work model, implemented a series of industry-changing actions that created immediate access to care. We also rapidly began delivering more than $9 million in support for affected communities and families statewide through our BlueCross Foundation.
The year 2020 proved to be our once-in-a-generation test to truly live our mission – in a by taking swift actions to enhance our ability to protect our members’ health, shield our own employees, and quickly and confidently choose the right thing to do – in a time of daunting challenge.
Our members always need us, but in 2020 depended on us more than ever. And combined with the national requisite for racial justice and healing, the need was great.
First Major Insurer to Lead with Telehealth
We became the first major insurer to commit to covering in-network telehealth services on an ongoing basis. In short time, by partnering with our providers, we saw 80 times more telemedicine claims than during the same period the previous year – an outstanding increase in access for our members.
Real Relief for Members, Groups and Providers
We made the decision early on to immediately waive member costs on COVID-19 testing and treatment until the end of the COVID-19 national emergency – whenever that may be. And later, for the approved and fast-tracked vaccines. We waived primary care and behavioral health costs for our Medicare Advantage members – those most vulnerable to the pandemic.
We also moved swiftly to assist our customer groups by extending payment periods to help their employees keep their critical group coverage – even as so many small businesses were facing difficult decisions about mass layoffs and closures.
And we honored and supported the front-line providers and first responders who worked tirelessly to deliver care round the clock.
Excelling in Member Satisfaction
Through the end of the year, our net promoter score continued to rise as our levels of service only increased during the challenging period. As an indicator of outstanding member satisfaction and loyalty, we’re working to be in the top quartile of performance for this key consumer service metric.
Taking the Right and Only Stand Against Racism
Though separated by distance, we joined together in our support of racial justice and healing, establishing internal conversations to make sure our employees had the opportunity to speak of their experiences, and taking the conversation public with a stake-in-the-ground stance against racism.
Our Mission is Our Guide
Throughout 2020, we took care with each decision to ensure it was the right thing to do for our members, our groups, and the providers we rely on to care for BlueCross members – to deliver peace of mind through better health, and an unqualified level of support in a defining moment of challenge and change.
JD Hickey, M.D.
President and CEO
Marty G. Dickens
Chairman of the Board

Making COVID-19 Relief a Reality
The health of our members, employees and the communities we serve was the first priority in 2020. Since the COVID-19 pandemic was unlike anything we had faced, our first decision was to remove any barriers to those needing and receiving care. We waived all member cost-sharing for COVID-19 treatments, including hospitalizations, in addition to waiving copays and cost-sharing for FDA-approved COVID-19 testing. No out-of-pocket costs were necessary for testing and treatment administered through in-network providers, including care at a doctor’s office, urgent care facility, emergency room, and COVID-19-related inpatient hospital stays.

As COVID-19 made its way to Tennessee, BlueCross took immediate steps to prepare for and respond to member and community needs, including supporting providers and first responders who placed their lives on the line every day. Our nurses and case managers took additional measures to ensure members had both their health and safety needs met – even arranging for food pantry and meal deliveries for those having financial difficulties.
BlueCross Foundation provided almost $9 million to support area food banks, sponsor provider education and COVID-19 vaccine education, address health disparities and encourage vaccine acceptance – especially in communities of color. And though in-person volunteer activities were suspended temporarily in 2020 due to COVID-19, TeamBlue volunteers still found ways to help their neighbors through our Community Trust outreach and engagement opportunities, making personal calls and check-ins on area residents as an additional way to give back to the communities where they live and work.
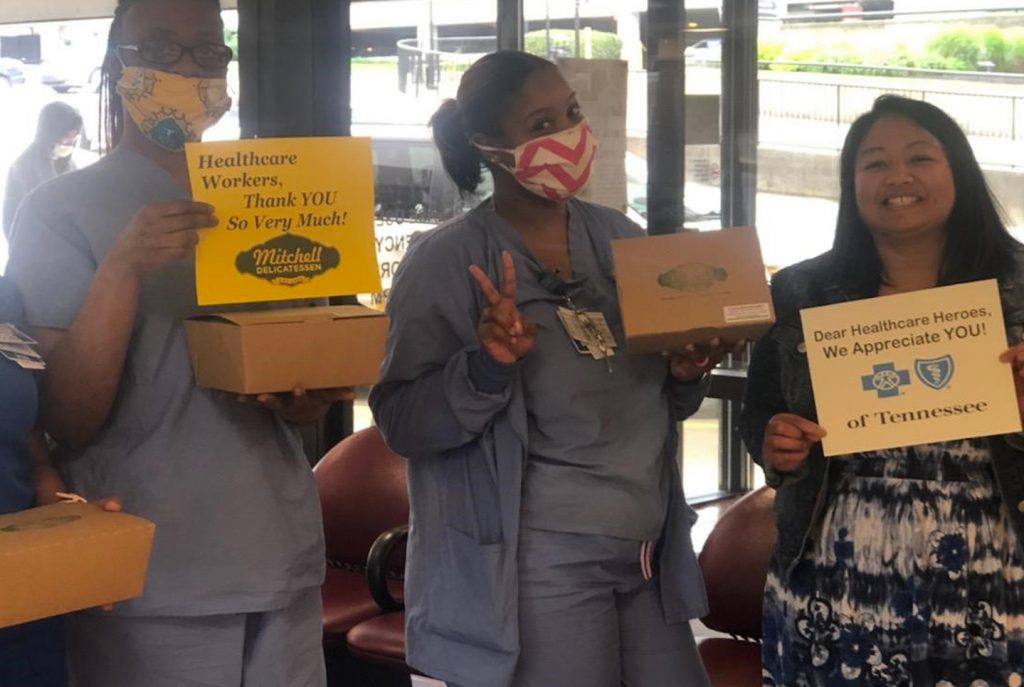
There were many ways to say thank you to the first responders and health care professionals who stepped up to the challenge and remained in action throughout the most difficult times of the coronavirus outbreak. BlueCross chose to thank and recognize the doctors, nurses, firefighters, police officers and EMTs for their life-saving work with public ad messages, social media support, and more than 6,500 yard signs that every employee could place in on their property. The signs and messaging – along with donating and delivering lunchtime meals to hospital work teams across the state – were a unifying way for BlueCross, our employees and volunteers, to visibly show support for these heroic efforts.

We became the first major insurer to embrace telehealth for the long-term after our dramatic expansion of these services during the COVID-19 pandemic. Strategically aligning with our commitment to improve access to primary care, our decision to permanently cover virtual visits with in-network providers gave members easier access and options to health care services moving forward. Our decision covered telephone and video visits with primary care providers, specialists, and behavioral health providers, as well as occupational, physical, speech, and ABA therapy services. Telehealth offers members and their trusted providers more options that fit their everyday needs for preventive, routine and maintenance care – driving better health.

Primary care is one of the best ways a person can pursue better health – and BlueCross BlueShield of Tennessee has a history of investing in successful, collaborative partnerships to elevate and ensure quality primary care for statewide residents. Our joint venture to open eight primary care clinics with Sanitas, a Keralty company, demonstrated an innovative way to fulfill our 2020 business priority to advance new models of care. Supporting and expanding convenient access to primary care, these medical centers in Middle and West Tennessee exclusively serve BlueCross members from all lines of business, along with self-pay and original Medicare members. Benefits of using our new clinics include same-day appointments, extended hours, and enhanced digital tools that make it easy to connect with care teams and medical center staff.

For the sixth year in a row, CMS recognized our Medicare Advantage PPO plan with a 4-Star quality achievement rating. Never easy to achieve, this industry accolade is based on up to 40 different performance measures, which are updated and weighted differently each year. Measures and calculation points can also change annually based on other Medicare Advantage plans’ performance across the U.S. – as well as CMS Stars program changes – so the bar continues to be raised each year. Four-Star rankings require consistent high performance across the entire structure of plan operations – with metrics designed to continually push plan programs for continuous improvement.

For all the progress made, the scars of deep-seated racism still exist. The disparities evident in COVID-19 outcomes and several tragic deaths over the summer turned our collective eyes to these issues with a new sense of urgency. We made a public statement to work to end racism and committed the company to better serve our communities in support of these specific needs. We funded new ventures and partnerships to research and address health disparities and hosted our most-attended Power of We workforce diversity conference to share best practices with business leaders across the state.

At the start of 2020, no one could have predicted that 97% of our employees would spend the next year working from their homes – or that we’d have to make the transition happen in a matter of days. Change has become the new normal and BlueCross BlueShield of Tennessee has adapted well to change over the past decade, as the competitive marketplace and regulatory landscape have evolved. Throughout, our enterprise strategy has focused on helping employees tie their roles and impact to our strategic goals, aligning our efforts while building agility and resilience. When faced with the need to balance the health of our employees and our commitment to member service, we were ready. In an unplanned era of remote work, our people have thrived – maintaining high levels of service, collaborating in new ways, and increasing our already-high engagement scores.

Starting in 1945, our organization’s purpose centered on access to affordable care and being good stewards of the health care dollar – guideposts we still follow. We continually add value for our customer groups and members, promoting evidence-based care and employing hundreds of nurses and other clinicians to assist our members and support their needs to achieve better health and a better quality of life. We’ve built a legacy of giving back to Tennessee communities. And to mark our 75th anniversary, our people used digital tools – ones our founders never could have imagined – to share photos, memories and perspectives on our mission. The common thread in all our efforts is the common good, which our people pursue by living these words each day: Peace of Mind through Better Health.

