Jameekah Bowling recalls a specific moment when she knew her team had made a difference in the life of a member.
“I went to a community event and met an older gentleman who a few weeks earlier thought he didn’t need a colonoscopy,” she says. “He was refusing it because he thought it was going to be too much of a hassle. But my team had called him, and we sent him what’s called an FOBT, or fit kit. His results were sent to his doctor, and it was later learned he needed some polyps removed.”
“When he introduced himself, he thanked me,” the operations supervisor on the senior care outreach team at BlueCross continues. “He said, ‘If it wasn’t for you all pushing me and telling me the fit kit didn’t hurt and was easy to use, I never would have called my doctor.’ That resonated with me, because all it takes is a gentle nudge from one of our specialists to help ensure we have a member who is going to be with us a bit longer.”
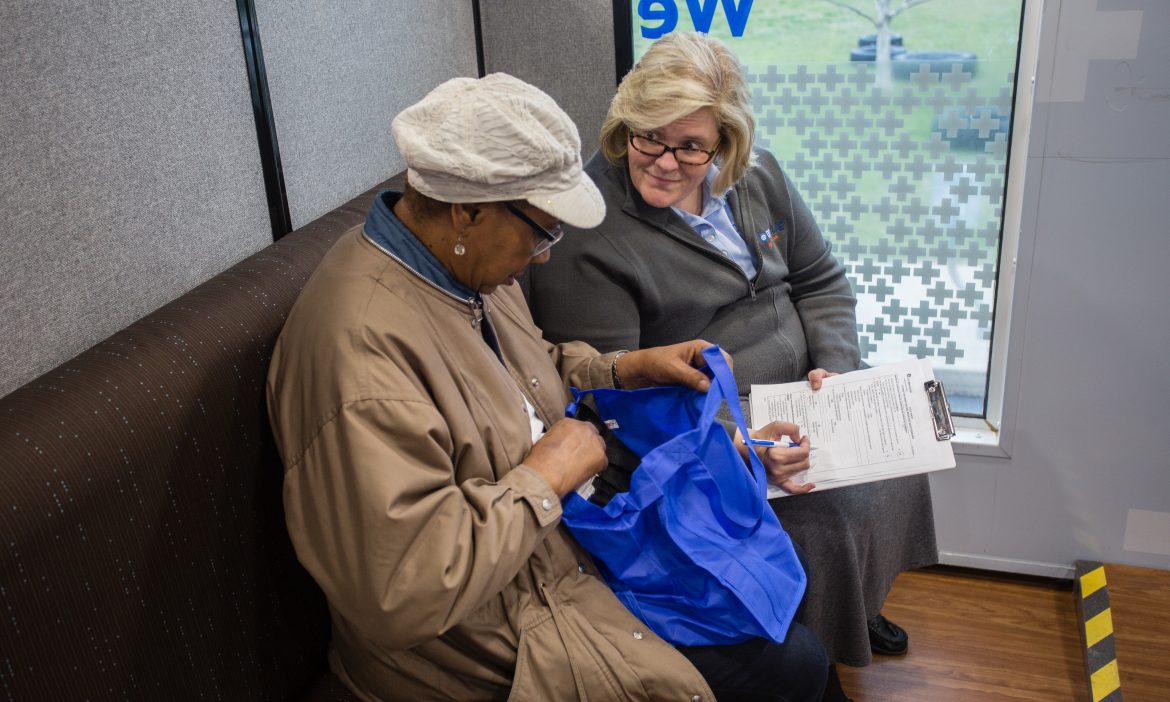
That experience was but one of the many times a representative from the senior care outreach team has “nudged” a member, which might as well be listed as part of the official job description. These stories are why we have a team of 30+ outreach employees providing services and support for our Medicare members.

A proactive approach
The team’s goal is to ensure members get recommended screenings and take their medications as directed. We accomplish this through:
- Member education – Representatives call members to educate them on why these screenings, such as a mammogram, diabetic retinal eye exam or colonoscopy, can help them stay healthy. From there, members are invited to one of our health and wellness events in their area or our team offers to schedule appointments for these services with a local plan provider.
- Pharmacy technicians – Certified pharmacy technicians call members to stress the importance of taking their medication as directed. If we see they’re not refilling their prescriptions, a pharmacy technician will call just to check in. It may be that the member only has a 30-day supply that has run out, so the pharmacy technician may provide education about the benefits of receiving a 90-day supply by mail.
- Connecting members to primary care physicians – These calls involve inquiring about whether or not a member has a primary care doctor. If so, we encourage the member to schedule an appointment if needed. If the member doesn’t have one, we can look up providers in their area who are part of our network, and recommend one to see.
“The member health and wellness events are especially important to build relationships and trust with these members,” Jameekah says. “We understand it’s hard for some members to get to a doctor’s office. There are a lot of rural areas in Tennessee, and it can be difficult for providers to travel to residences to provide preventive health services. So when we call about an event, we stress that, ‘We’re in your area, and we want you to complete your preventive screening so you can stay healthy and have a peace of mind, as well.’”
Connecting the communication dots
The goal of the senior care outreach team is to help members realize we are here to help and make screenings and medication as convenient and comfortable as possible for them. For example, representatives frequently educate members about screenings such as mammogram and colonoscopy being less invasive than in decades past.
In these instances, transparency is key.
“A call from an insurance carrier can seem overwhelming at first, so we let these members know who we are and why we’re calling within the first few seconds,” says Destiny Gordon, manager of outreach services at BlueCross. “Otherwise, you’re not going to get their buy-in.”
“With the senior population in particular, someone from somewhere is always calling about something,” Destiny adds. “We don’t want to be just another unexpected call they had to field that day.”
“We also let them know that they may get a follow-up call from another team member in a couple of weeks to check on their progress.”

Outreach team representatives also aren’t afraid to offer up their stories, when relevant.
“We have specialists who relate to members by sharing their truth,” Jameekah says. “Sometimes that’s a story about how a 3-D mammogram detected a lump, leading to lifesaving treatment. Or how they were pleasantly surprised themselves by how easy the process was. ‘Things are different than what they were 10 years ago. It’s a different machine. It doesn’t hurt.’ Our specialists take that extra step.”
“Opening up to a stranger can go a long way and show that this is not an automated call, but ‘This a person who has called me and is willing to share a piece of themselves in the interest of me being healthier.’”
Recognizing member preferences
The senior care outreach team’s efforts involve more than just phone calls. The team is strategic in its approach, asking members when they sign up for Medicare about their contact preferences. Sometimes their efforts involve a reminder postcard, other times all communications moving forward are digital. That has meant getting past preconceived notions about how seniors use technology.
“The members who are aging in to the Medicare Advantage program are much savvier than even five years ago,” Destiny says. “In 2018, we’ve seen three times the amount of digital engagement than before. A lot of that comes with the education at our health and wellness events. Our team attends these events and can help members set up the MyHealthPath app on their smartphones.”
“We’ve found that these members want to be digitally engaged – they just don’t always know how to be.”
While defining success for the senior care outreach team is easy – Medicare Advantage members adhere to their medications and receive recommended preventive health screenings – the methods to achieve this success are anything but. Moments like the one in Jameekah’s story demonstrate how members benefit from these services. And those moments always begin with a simple step – and a familiar refrain.
“We nudge,” Jameekah says. “We nudge, and we educate.”
 Jesse joined the BlueCross BlueShield of Tennessee corporate communications team in 2017. A Chattanooga native, he has more than 15 years’ experience in content creation, management, and strategy for consumer audiences, including a six-year stint in health care marketing.
Jesse joined the BlueCross BlueShield of Tennessee corporate communications team in 2017. A Chattanooga native, he has more than 15 years’ experience in content creation, management, and strategy for consumer audiences, including a six-year stint in health care marketing.