BlueCross BlueShield of Tennessee is a mission-driven, not-for-profit health plan founded in 1945. Today, we serve 3.4 million people across the state and around the country.
Here are a few fast facts about BlueCross:
- Taxpaying, not-for-profit company established more than 75 years ago
- Serving 3.4 million members and 11,000 companies as the state’s largest health plan
- Partnering with 54,000+ health care providers
- Giving $10 million each year in charitable investments
- Employing 6,500+ professionals to fulfill this mission:
Peace of Mind through Better Health
How BlueCross performs
Learn more about our corporate performance, community impact, and diversity efforts by downloading our annual reports.
- 2022 Diversity & Inclusion Report
- 2022 Financial Performance Overview
- 2021 Annual Report
- 2021 Financial Performance Overview
- 2020 Annual Report
- 2020 Financial Stewardship Overview
- 2020-2021 Diversity & Inclusion Report
- 2019-2020 Diversity & Inclusion Report
- 2019 Annual Report
- 2019 Financial Stewardship Overview
- 2019 Diversity & Inclusion Report
- 2018 Diversity & Inclusion Report
- 2018 Annual Report
- 2018 Financial Stewardship Overview
- 2017 Annual Report
- 2017 Financial Performance Overview
- 2017 Diversity Annual Report
- 2016 Annual Report
- 2016 Financial Performance Overview
- 2016 Diversity Annual Report
- 2015 Diversity Annual Report
- 2015 Annual Report
- 2015 Financial Summary Report
- 2014 Annual Report
- 2014 Diversity Annual Report
In 2022, we used 88 cents from every premium dollar to pay for our members’ medical needs.
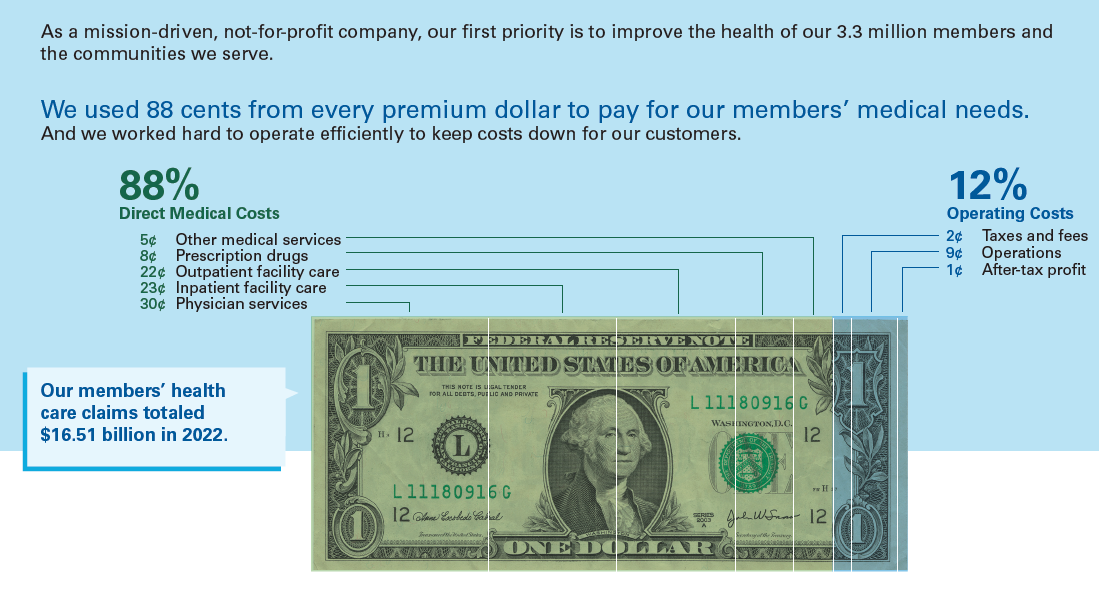
Download the full infographic about our financial stewardship in 2022.
We’re a taxpaying not-for-profit, which allows us to earn lower margins but also brings a responsibility to maintain strong reserves.
Our 3.4 million members want and expect us to perform well operationally and financially. They want to know we have the financial means to cover health care claims regardless of the economy’s ups and downs. We’ve built our reserves over 75 years to provide peace of mind to our members.
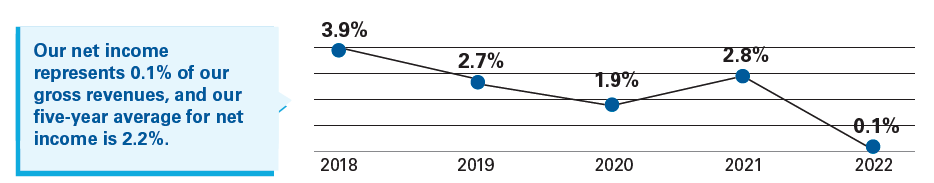
As a mission-driven not-for-profit, we have a unique ability to earn smaller profit margins – averaging 2.2% over the past five years – and a responsibility to maintain healthy reserves. This is especially important because we don’t have access to capital markets and cannot raise funds on an as-needed basis.
The Tennessee Department of Commerce and Insurance requires that we maintain $2.6 billion in reserves to ensure BlueCross and its subsidiaries could pay all claims and sustain business, even in case of emergency, disaster or cyclical downturn of business. We have an additional $1.5 billion in unassigned reserves.
- 40 – the number of days that BlueCross’ minimum required reserves could cover members’ claims
- 113 – the number of days that BlueCross’ total reserves could cover members’ claims

