Key Takeaways
- BlueCross BlueShield of Tennessee (BlueCross) paid out a record-high $16.76 billion in claims, including $1.1 billion for COVID-19 testing and treatment.
- 88 cents from every premium dollar paid for drugs and medical services on behalf of our members.
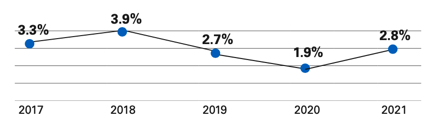
- After-tax income was just 2.8% of gross revenues, and more than half of our net income came from investments, rather than operations.
As a mission-driven, not-for-profit company our priority is to improve the health of our 3.3 million members and the communities we serve. That starts with providing affordable access to quality health care, and ensuring we pay our share of your health care costs quickly.
We did that in 2021, paying out a record-high $16.76 billion to meet the health care needs of our members.
As we look back on record-high claims costs there’s a renewed urgency to respond to our members asking us for greater affordability.
One way we work to lower costs is by consistently monitoring our networks to make sure we’re delivering the right balance of access and affordability. In some cases, by focusing members’ choices of health care providers, we can help deliver better prices. But we’ve also expanded in-network telehealth offerings and helped launch eight new BlueCross Medical Centers, operated by Sanitas, just for BlueCross members in Nashville and Memphis. Additionally, hundreds of thousands of BlueCross members used telehealth services in 2021, and we remain committed to promoting this convenient, affordable care option.
At BlueCross, we value the opportunity to bring peace of mind to our members by providing them with access to care that otherwise may be out of reach.
Being mission-driven also means we have a responsibility to be open about how we use your money. Here’s how our business performed in 2021 and what it means to you.
Breaking down the dollar
We used 88 cents from every premium dollar to pay for our members’ medical needs.
2021 Premium Dollar

What did we pay out for different kinds of care?
- 27 cents: health care services provided by a licensed medical physician
- 25 cents: inpatient facility care
- 22 cents: outpatient facility care
- 8 cents: prescription drugs
- 6 cents: other medical services
And we worked hard to manage operating costs effectively to keep costs down for Tennessee-based employers and our members.
After paying for our members’ care, we:
- Paid out 2 cents in local, state, and federal taxes
- Used 8 cents to run our business operations
- And had 2 cents left as net income, or profit
The pandemic led to major economic disruptions that affected our customers and members – and therefore our business as well.
Throughout 2021, we focused on removing barriers to care and supporting members and communities through the COVID-19 pandemic. In 2021, we distributed $1.1 billion to pay for members’ COVID-19 care. That’s up from $738 million in 2020, a 49 percent increase.
We paid $451 million in taxes that support programs and services benefitting Tennesseans, and we earned $521 million in after-tax net income. 62 percent of our net income came from investments, rather than operations.
As we shared above, we’re good stewards of our premium dollars. And separately, our foundation committed $16 million to support communities across Tennessee funding disaster relief, education scholarships, COVID-19 vaccine education and distribution, and establishing 10 BlueCross Healthy Places mostly in rural communities across the state.
Our 2021 net income represents 2.8 percent of our gross revenues, and our five-year average for net income is 2.9 percent.
We are a taxpaying not-for-profit, which allows us to earn lower margins but also brings a responsibility to maintain strong reserves — as demonstrated by the challenges many businesses faced due to the COVID-19 pandemic.
Any net income we earn goes into our reserves or gets invested to enhance our member service capabilities. So, our 2021 financial performance allows us to stay strong for our customers, as demonstrated by our A+ Stable rating from Standard and Poor’s.
Our required reserves would cover our members’ claims for 68 days. We have $414 in additional reserves per member, which would cover another 38 days of claims.
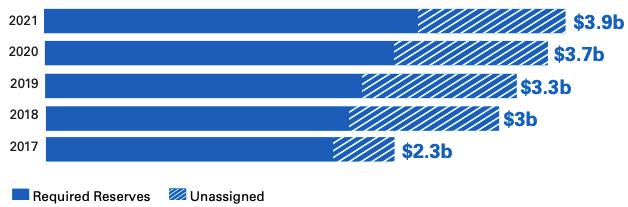
Our reserves — built over 75 years — now total $3.9 billion. $2.5 billion of those are required based on how many members we have and how much we must charge in premiums. Reserve requirements rise alongside the cost of medical care and services.
We believe it’s critical to hold those additional reserves — and our current national emergency shows how unforeseen events can affect the economy and our business.
Responding to customer demands for affordability
Our customers have always asked us to help manage their costs, but their expectations are more urgent than ever.
One powerful tool to deliver cost savings is our provider networks.
Provider networks:
- Bring more patients to those providers in exchange for discounted rates
- Help us make sure the providers are meeting safety and quality standards
We’re reviewing our provider networks to determine how we can deliver the most value for businesses like yours, and for our members. At the same time, though, the Wall Street Journal reports that hospitals want to raise treatment costs.
Since improving affordability for everyone is our goal, we’ll keep working to negotiate the best possible rates with hospitals and providers.
Our teams are carefully evaluating every opportunity on the table to make sure we are meeting the expectations of customers. We are excited to take on this challenge, and we will use every tool we have to deliver on quality and affordability in 2022 and beyond.
Glossary
- Claim: A request for payment that you or your health care provider submits to your health insurer when you get items or services you think are covered.
- Premium: The amount you pay for your health insurance every month. In addition to your premium, you usually must pay other costs for your health care, including a deductible, copayments, and
- Gross revenue: the sum of all money generated by a business, without considering any part of that total that has been or will be used for expenses.
- Net income: the amount an individual or business makes after deducting costs, allowances, and taxes.
- Network: The facilities, providers, and suppliers your health insurer or plan has contracted with to provide health care services.

