Originally published in The Tennessean, October 2023
Imagine you’re a recently retired 68-year-old on a fixed income and in need of a health insurance plan. Perhaps you retired a few years after the eligibility age of 65, working a while longer to secure your nest egg, but are now overwhelmed by the coverage choices available to you.
You’re not alone. With the Medicare annual enrollment period open now through December 7, navigating the field of available options can be difficult — and not just because of today’s fluctuating economy and financial uncertainties.
You’ve likely received several health plan fliers and offers from different carriers, and every trip to the grocery store has billboards with competing plans seeking your business.
Picking the right plan for you
When people become eligible for Medicare, choosing a plan shouldn’t be a burden — especially as we get older and face more complex health challenges. Having been with BlueCross for a little over a year now, my role involves making sure our Medicare Advantage members have a positive experience when selecting and using their benefits, connecting with the right providers, and getting high-quality care. But what’s most rewarding for me is how we’re constantly looking at ways to take stressors off the table.
We do so by listening to our members and evaluating our operations to better serve them — and changing our product offerings to meet the evolving health needs of Tennesseans and their ability to lead active, healthy lives.
Seniors choose our Medicare Advantage products due to the high degree of service and provider access we’ve created to coordinate care.
My team works alongside providers and members to find ideal ways to help improve health outcomes. This work includes partnering with providers to better document Medicare Advantage members’ care and health status and supporting other workflow improvements for the overall care experience. One such strategic partner is Ascension Saint Thomas in Nashville, who has been a high-value provider in our network for many years.
New ways we’re connecting with our members
Part of our evolving strategy involves recognition of health challenges and working closely with BlueCare Tennessee, a subsidiary of BlueCross BlueShield of Tennessee. BlueCare was selected by the state to help manage its Medicaid program. We’ve bridged a gap by creating BlueAdvantage Extra, a plan ideal for members who are receiving some state assistance but not enough to qualify for a Dual Eligible Special Needs Plan (DSNP). One appealing aspect of this new plan is the inclusion of a transportation benefit to help members get to and from their medical appointments.
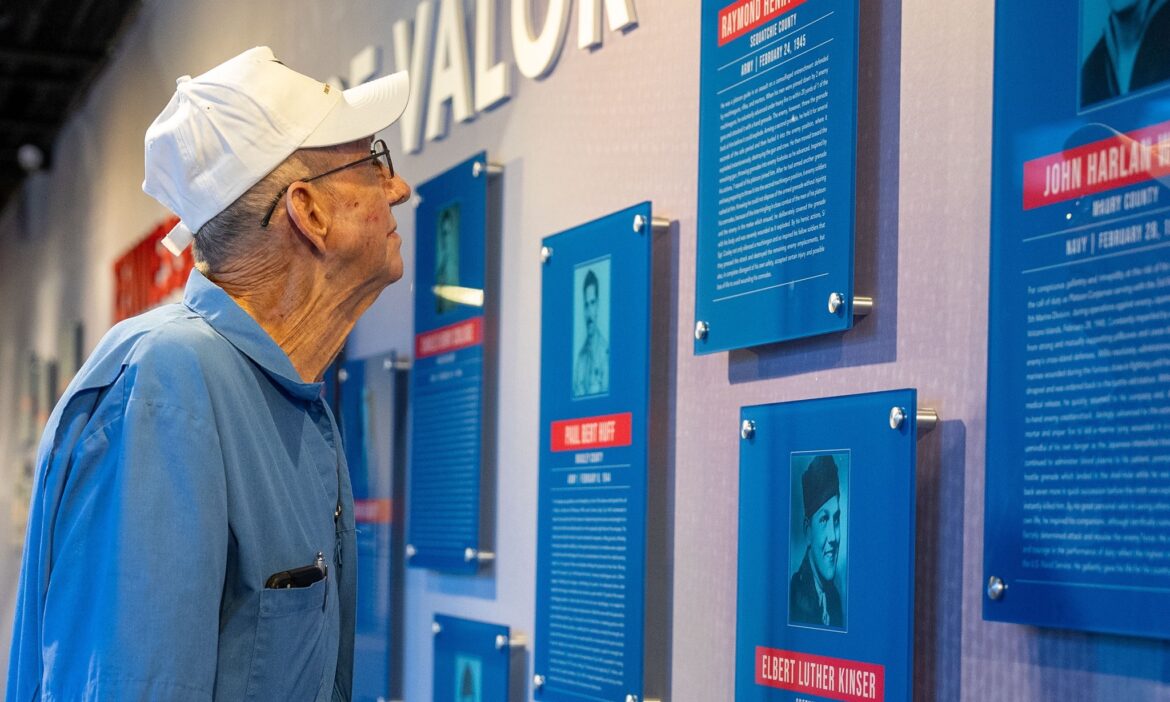
We’ve also built on our strategy to reach veterans and enroll them in our plans by communicating with them directly.
Efforts such as this show why our Medicare Advantage PPO plan recently earned a 4.5 out of 5-Star quality rating from the Centers for Medicare & Medicaid Services (CMS), marking the third consecutive year we’ve scored 4.5 or higher. The BlueCross Medicare Advantage PPO plan also earned high rankings in customer service and member outreach.
What brought me to BlueCross just over a year ago was its compassion for its members and how we keep their best interests in mind when creating benefit packages and rolling out support programs. It’s gratifying to see that recognized by CMS, as we know our teams’ efforts and outreach to members make a positive difference in the quality of care they receive.
But we’re also here to help facilitate conversations between our members and their providers. Each individual is their own greatest advocate.
For those considering or actively seeking a change in coverage, it’s vital to talk with your provider about your options as your health needs change.
You can find more information about Medicare plans here or by visiting Medicare.gov’s Plan Finder.

 As Medicare general manager, Jason is responsible for overall performance and management of all Medicare Advantage and Medicare Supplemental product lines.
As Medicare general manager, Jason is responsible for overall performance and management of all Medicare Advantage and Medicare Supplemental product lines.