When a change is necessary, sometimes all you need is a push in the right direction.
Dawna Baird, a 40-year-old member in northeast Tennessee, had a history of health challenges and a desire to improve her overall wellbeing. Earlier this year, her conditions, which include Type 2 diabetes, drew the attention of a BlueCross care coordinator.
The care coordinator, who worked onsite at Dawna’s primary care practice, reached out to her about finding ways to meet some of her wellness goals.
“I shared that I wanted to change how I eat and manage my stress,” Dawna recalls.
“My care coordinator told me about the CareTN app and digital care management programs that would help me manage my diabetes more effectively and provide mental health support to lower my stress level, so I decided to participate.”
In the months that followed, Dawna focused on improving her physical health and eating habits first. She successfully completed the online diabetes care program through the CareTN app and met virtually with her BlueCross support team, which included the care coordinator and a registered dietitian who provided additional education, guidance and encouragement.

“I had daily and weekly check-ins via the app so my team could see how I was doing, and we could chat via instant message if any questions or roadblocks came up,” Dawna says. “The app included an automatic step tracker and goal tracker which was really nice. It would send me reminders to take my medications, as well as encouraging notifications, like ‘This week, you want to be working on x, y, and z in order to get where you want to be.’”
When Dawna returned to her primary care physician, he was thrilled with her progress. In the course of the program, she lost 30 pounds and improved her blood sugar considerably.
Dawna still uses the app to track her steps and reach out to her care coordinator when needed, and she is working to maintain her momentum.
“Seeing members like Dawna move through these programs so quickly and with so much thirst for knowledge to improve their chronic conditions and overall health is inspiring,” says Sabrina Logan, provider programs manager for BlueCross.
“We’ve seen that this type of support can make a huge difference in quality of life, and that’s definitely true in Dawna’s case.”
For her stress management goal, BlueCross connected her with a behavioral health case manager who guided her to another digital program designed to provide education and guidance. The in-app library of tools and articles on best practices for managing stress proved helpful for Dawna.
As before, if she had any questions or needed extra motivation, her care coordinator was only a few keystrokes away.
“It’s made getting healthy much easier,” Dawna says, “because I had all that support available anytime on my phone.”
Dawna is one of thousands of Tennesseans being served by the Medical Home Partnership (MHP), the latest BlueCross program designed to improve our members’ overall wellbeing and address health care cost increases through effective collaboration with health care providers.
Evolving provider partnerships provide better care
The roots of MHP go back more than a decade as BlueCross focused on finding new ways to partner with providers to support better health for members. That began as we developed a system that rewards the value of the care provided — not just the quantity of services a patient receives. Over the years, the BlueCross value-based care effort has helped many members overcome challenges to build healthier lives for themselves.
The first part of this effort, known as the Patient Centered Medical Home, was created in 2009 to provide extra support for our members with certain chronic conditions such as diabetes.
The next phase of our value-based care evolution came in 2015 with the launch of the Quality Care Partnership Initiative, or QCPI. This program built a network of primary care providers who have agreed to be paid based on the quality of the health care they provide our members as measured by health outcomes and overall care experience.
In 2020, BlueCross took another step forward by establishing the MHP.
This program’s participating providers, all of whom are already part of QCPI, make it easy for members to seek care with extended hours for appointments, phone and email consultations, and online portals for viewing test results and messaging with doctors. Many participating providers also offer urgent care services.
Perhaps most importantly, MHP practices have BlueCross care coordinators like Heather helping primary care providers identify member needs and provide the right level of outreach to address any issues.
Making a difference for members
Results so far have shown the MHP approach makes a difference.
BlueCross members who receive care from providers in the MHP program are reporting positive care experiences, achieving better health outcomes, and are less likely to receive unnecessary care.
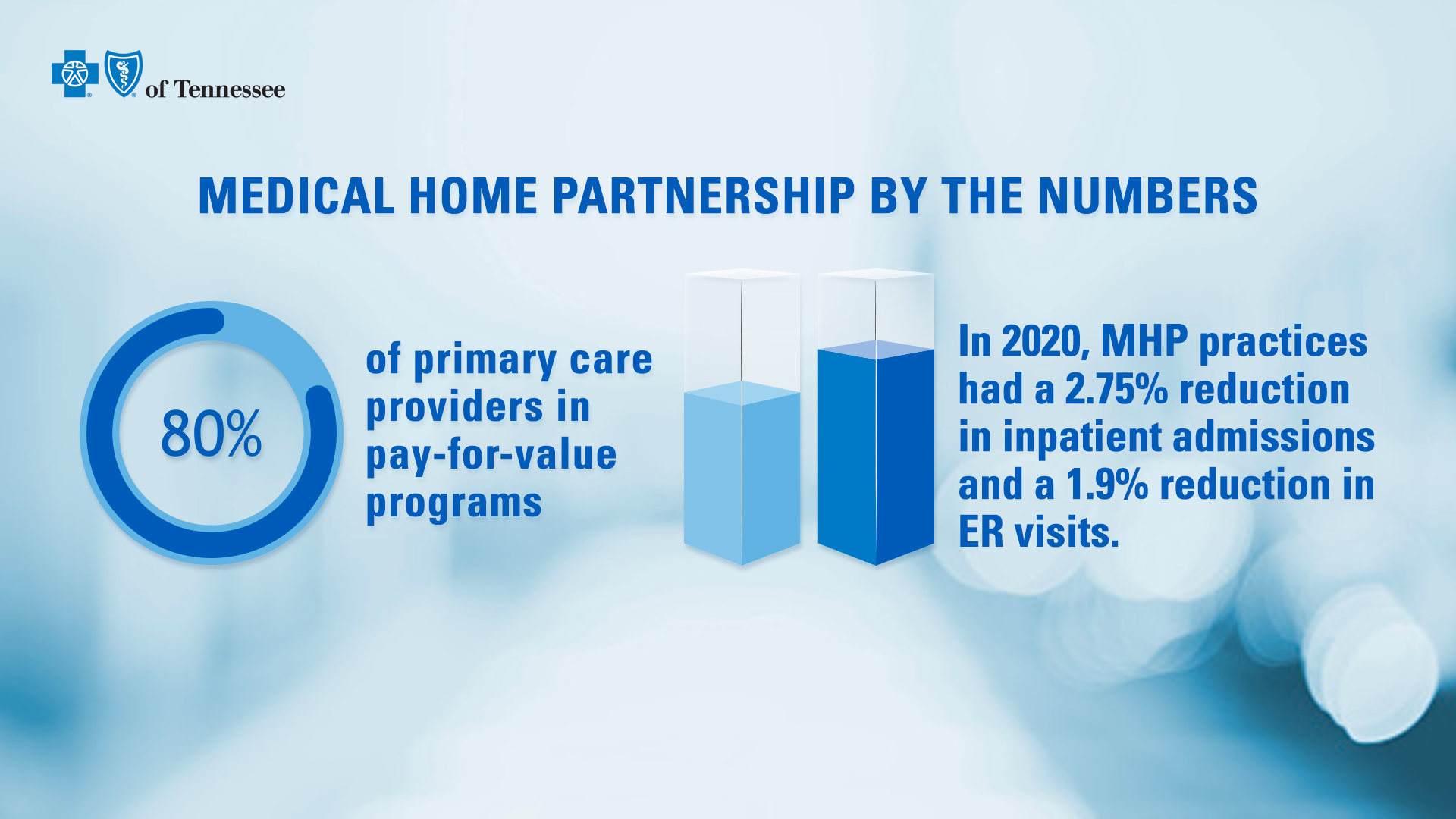
The approach is expanding: today, more than 80 percent of BlueCross in-network primary care physicians participate in a pay-for-value program. Compared with the competition, BlueCross has three times as many providers in value-based programs.
And the positive impact of these programs is clear. Even during the pandemic, MHP providers have had fewer members visit the emergency room or end up as hospital inpatients compared to traditional primary care providers.
In 2020, a review showed that the MHP practices had higher quality scores than their non-MHP counterparts, which shows their care was more effective. A 2020 program evaluation showed that for every dollar invested in MHP, more than $4 has been saved, mostly thanks to fewer ER visits and inpatient hospital admissions.
This savings reduces claims costs, which in turn reduces premium increases for employer groups and members.
State of Franklin Healthcare Associates (SoFHA) in northeast Tennessee is currently the top performing practice in the MHP program.
“The rewards we’ve earned for high performance in the MHP program have helped us grow our Quality Improvement Team, which includes registered nurse case managers, social workers, and clinical pharmacists,” says Dr. Rick Moulton, an internist and quality leader at SoFHA. “This growth will enable us to provide more outreach to chronic and complex patients.”
“As we reinvest these rewards, our efficiency and patient experience improve. This keeps the group moving in the right direction to effectively address care, health, and cost in the system.”
For their part, BlueCross innovation leaders are grateful for the chance to support and extend the efforts of clinicians to provide the best possible health care.
“We’re proud of the connections we’ve built with these providers, and the true value of the care we’re able to offer members,” says Allison Scripps, director of operations for BlueCross Quality Care Partnerships. “Ultimately, it’s all about what we’re able to do for the people we serve.”


 Alison has been a member of the BlueCross BlueShield of Tennessee corporate communications team since 2015. A Chattanooga native, she has a decade of health care communications experience including writing, editing, public relations and social media.
Alison has been a member of the BlueCross BlueShield of Tennessee corporate communications team since 2015. A Chattanooga native, she has a decade of health care communications experience including writing, editing, public relations and social media.